Abstract
Introduction: The recent pandemic brought to light the fragility of the US Blood Collection system and supply chain disruption. As blood donations declined, blood donor centers (BDC) and blood banks (BB) worldwide reported a significant blood shortage. Our blood donor center had challenges from imposed COVID precautions (social distancing, contact restrictions, donations by appointments only, wearing of PPEs, etc.) to increase blood collections to replace the units transfused daily. The study was to review our Institutional process for development of Covid-19 risk levels-based dashboards which tracked the pandemic and provided risk levels in real time to faulty/staff employees.
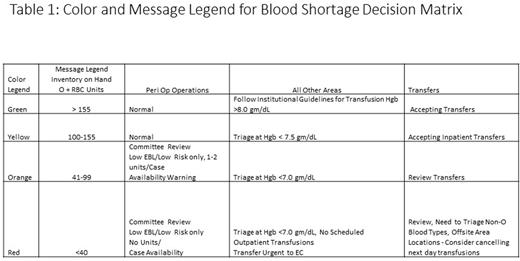
Methods: As the Blood Inventory decreased daily during the start of the pandemic and ultimately became critical, the Transfusion Service/Blood Bank (TS/BB) would reset and lower the triage Hgb level from 7.0 gm/dl to 8.0 gm/dL based on O pRBC units in inventory. The challenge was to disseminate the blood inventory to all stakeholders, decrease the number of calls/pages to TS/BB/Transfusion Medicine Physician (TMP) on call and be consistent in setting Hgb triage levels. Surgery/Anesthesia required daily inventory to predict cases that would have to be cancelled and rescheduled for possible increased estimated blood loss. As the national/local blood supply shortage became critical especially for O RBC Units, a Blood Shortage Decision Matrix was created in collaboration with our Chief Patient Safety Officer, Chief Administrative Quality Officer and Chief Information Technology Officer teams with a color-coded legend (RED - Hgb <=7.0 gm/dL [Emergencies only], ORANGE- Hgb <=7.0 gm/dL, YELLOW -Hgb <=7.5 gm/dL and GREEN <=Hgb 8.0 gm/dL) illustrating how blood would be triaged based on the O red cells units available in Inventory for transfusion each day (See Table ). Minimal/critical numbers for each blood product/blood group were derived based on logistic regression/machine learning/manual counts from historic usage within the past 2 years. A similar color-coded diagram was used for Platelet Inventory. The blood inventory continues to be reported at the daily morning Department/Divisional (Operations) Tier Readiness Briefings (Institution's Pathway leading to a High reliability Organization) for institution wide dissemination.
The TS/BB Information System is linked to real time blood inventory of all blood products entered into the system and provided us with real time inventory except for units that required a second ABO Rh and irradiation. Computer queries were performed for the latest inventory by blood product available and received, total number of Inpatient and Emergency Medicine patients by blood types and their latest hemoglobin values with transfusion orders and transfused currently, patients who were not transfused currently with no active orders and patients who were transfused since last day of transfusion by blood types.
Supply Estimates were made for blood products from donors collected at our BDC and blood products that would have to be purchased from outside suppliers. This was to guide decision making for both the BDC to provide blood products to the TS/BB and for the TS/BB to assess how many products needed to be ordered from outside suppliers. Demand estimates were made from historical data, current inpatient census from the EMR inpatient dashboard, number of current inpatients (ICU, Hematologic Oncology, Acute Cancer Care Center etc.) who were O pos (Per Webi query with a real time report run each morning), by location, blood type, hemoglobin level and days since latest hemoglobin level. Data was used to assess how many of the patient groups already met hemoglobin levels designed by the color code chart described above between 7.0 and 8.0 gm/dL which assisted the TS/BB to triage pRBC orders based on Hgb levels set for the colors.
Results: The Blood Shortage Decision Matrix since its implementation in October 2021 has allowed clear organizational-wide ownership across all levels of the organization, use of a standardized Blood Inventory management by the TS/BB, improved communications with primary care teams, better understanding of the challenges maintaining an adequate blood supply by the Executive/Administrative Leadership leading to allocation of additional needed resources to the Blood Donor Center/TS/BB and also helps the Institution on its path toward a High reliability Organization.
Disclosures
Aung:Helena Lab: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal